mintek.co.za
Introduction GOLD 2006 PRESENTATION Tertiary bis-phosphines of the form R P-(CH ) -PR (n = 1 – 4 and R = Me, Et, t-Bu and Ph) and cis-R PCH=CHPR (R = Ph) are often used as chelating ligands for a wide range of transition metals.[1-4] These ligands have shown wider applications in metal complexation reactions and have attracted much attention, especially in the fields of medicine and cat
 Noninvasive home ventilation Budweiser et al.
Noninvasive home ventilation Budweiser et al.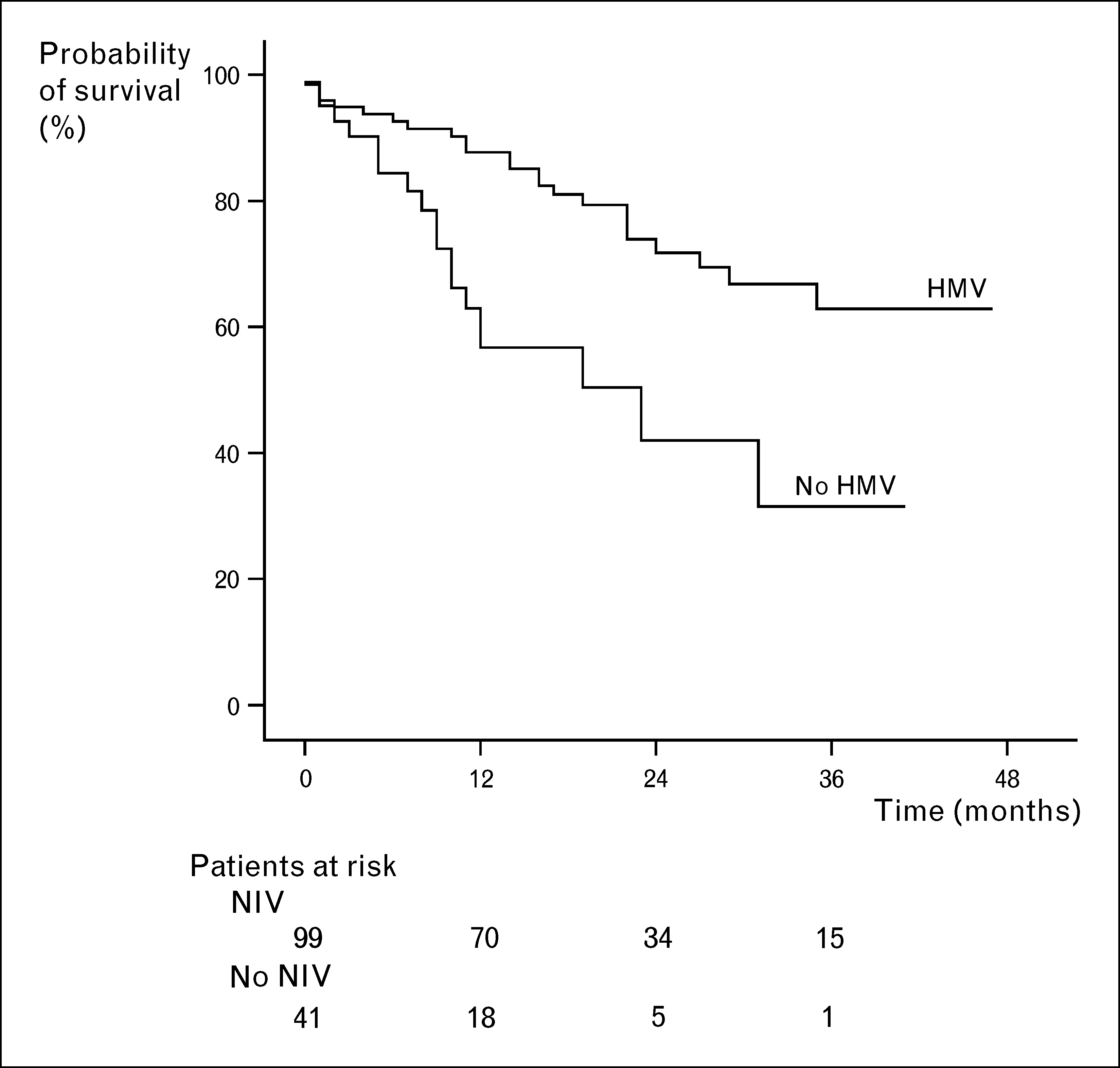 Obstructive, occupational and environmental diseases
which was recently also validated specifically for COPD
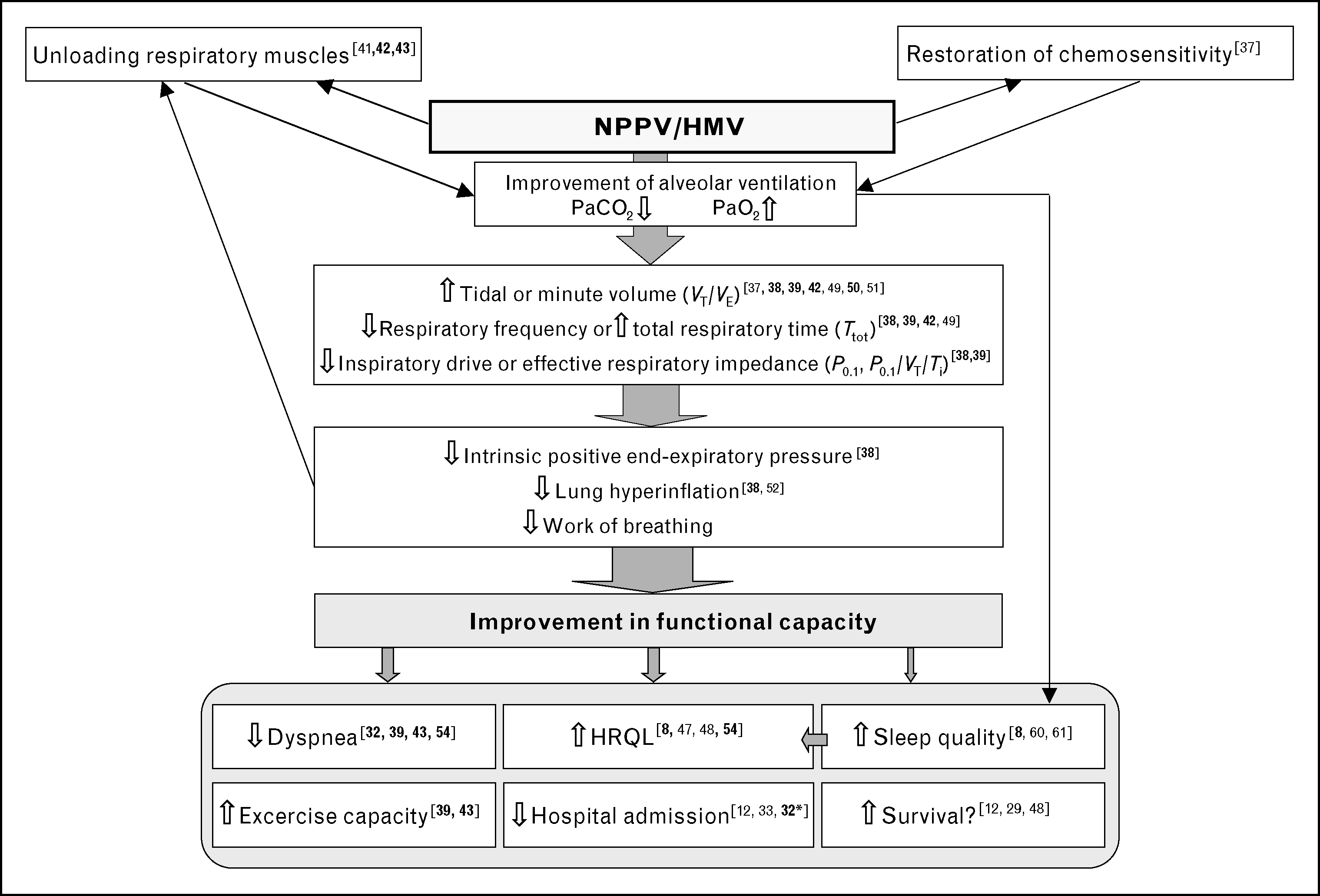
In view of the potential of domiciliary noninvasive venti-
lation to reduce overall healthcare costs, at least inpatients with recurrent exacerbations HMV should
Contrary to the predominantly favorable findings regard-
thus be further evaluated in randomized controlled trials
ing HRQL, the two randomized clinical trials on long-term
and samples of adequate size. As suggested factors
mortality which comprised samples of acceptable size and
in favor of an improved long-term outcome are the
observation periods of 1 and 2 years, respectively, found no
selective inclusion of patients with severe COPD and
difference in survival rate between patients with HMV
high risk for exacerbation or death, sustained adaptation
compared to LTOT alone Treatment efficiency
to HMV, high pressure levels, and familiarization with
and inspiratory pressure levels might, however, have been
the technique. Naturally, HMV can only be part of a
too low Although changes in overall treatment
comprehensive management strategy in COPD and
associated with HMV should be taken into account, it
should be noted that survival rates of patients treated with
pharmacological therapy and LTOT Even in the
noninvasive efficient HMV were higher than those of
terminal stage of the disease noninvasive ventilation can
historical controls In a further observational
alleviate symptoms without the undesirable side-
study comprising the as yet largest population and longest
effect of prolonging the process of dying.
Obstructive, occupational and environmental diseases
which was recently also validated specifically for COPD
In view of the potential of domiciliary noninvasive venti-
lation to reduce overall healthcare costs, at least inpatients with recurrent exacerbations HMV should
Contrary to the predominantly favorable findings regard-
thus be further evaluated in randomized controlled trials
ing HRQL, the two randomized clinical trials on long-term
and samples of adequate size. As suggested factors
mortality which comprised samples of acceptable size and
in favor of an improved long-term outcome are the
observation periods of 1 and 2 years, respectively, found no
selective inclusion of patients with severe COPD and
difference in survival rate between patients with HMV
high risk for exacerbation or death, sustained adaptation
compared to LTOT alone Treatment efficiency
to HMV, high pressure levels, and familiarization with
and inspiratory pressure levels might, however, have been
the technique. Naturally, HMV can only be part of a
too low Although changes in overall treatment
comprehensive management strategy in COPD and
associated with HMV should be taken into account, it
should be noted that survival rates of patients treated with
pharmacological therapy and LTOT Even in the
noninvasive efficient HMV were higher than those of
terminal stage of the disease noninvasive ventilation can
historical controls In a further observational
alleviate symptoms without the undesirable side-
study comprising the as yet largest population and longest
effect of prolonging the process of dying.