Prinzess
WIE MAN(N) EINE PRINZESSIN WIRD © Copyright Cheryl Ann Costa 1994. All rights reserved. © Copyright der deutschen Übersetzung Thespis-Verlag, 1999Dieses Stück kann entweder als Monolog oder als Einakter umge-In der Version als Einakter gibt es Teile eines metaphorischenMärchens vor jeder Szene, welche in der Monolog-Version wegge-lassen oder eingangs als ganzes Märchen erzählt werde
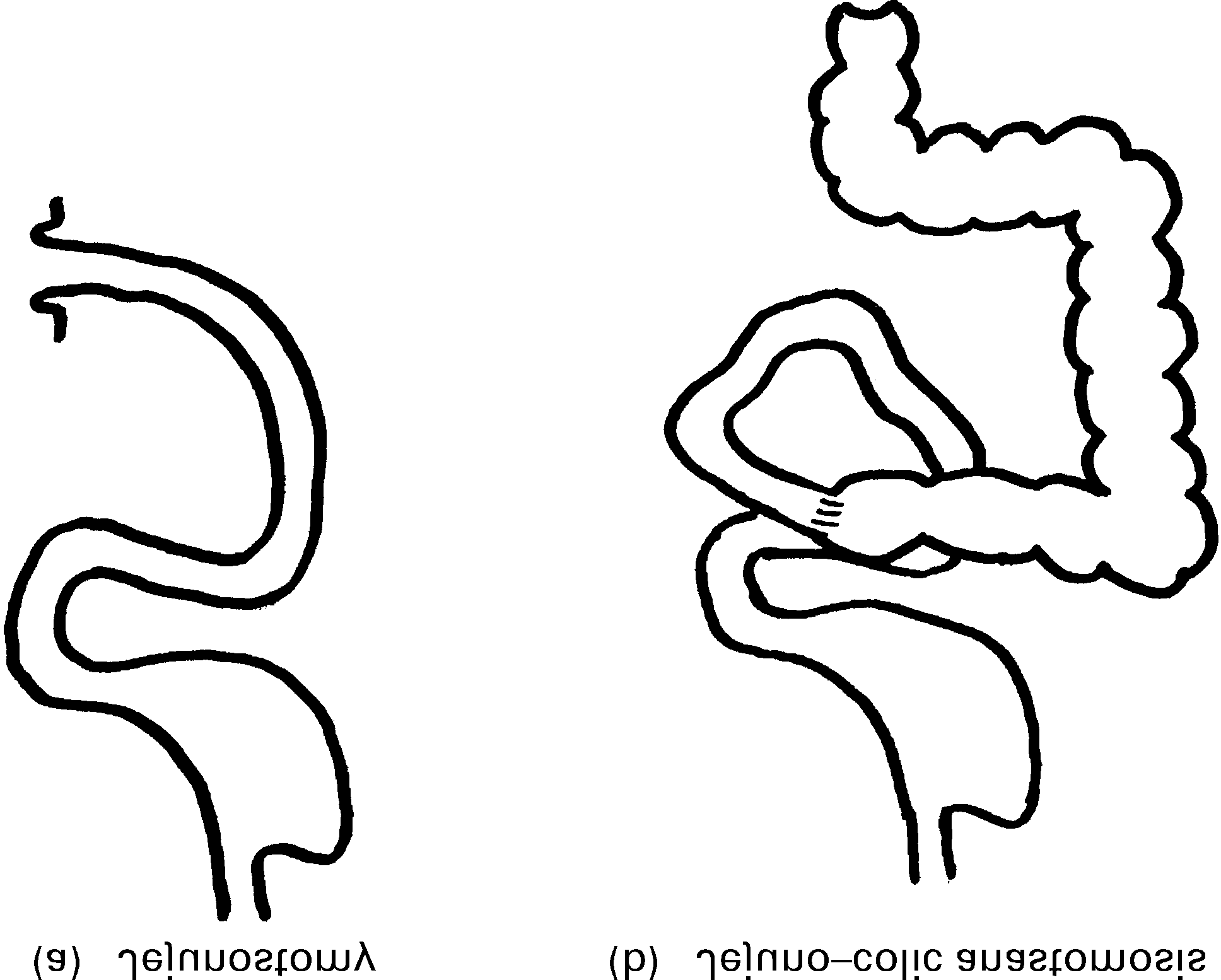 Methods for reducing the severity of chronic intestinal
Methods for reducing the severity of chronic intestinal